Why is it important to recognize when I have experienced significant trauma? How can one recover from the paralyzing effects of a traumatic event? How can knowing Jesus can make a true lasting difference?
What is Trauma?
Clinical definition: “Trauma is the response to a deeply distressing or disturbing event that overwhelms an individual’s ability to cope, causes feelings of helplessness, diminishes their sense of self and their ability to feel a full range of emotions and experiences.”
Who does trauma affect? Everyone. Yes there are groups of people who experience trauma more regularly, whether it is a helping profession or certain demographics, but trauma can affect all of us. Trauma does not discriminate no matter your socioeconomic status, sexual orientation, gender, race, whatever.
Facts about Trauma:
70% of individuals in the USA will encounter at least one traumatic event. Personally I think this may be higher, but this is what research says.
There are 3 types of trauma:
– Acute: Acute trauma results from a single incident; a one-time event that happens to someone, such as a car accident.
– Chronic: Chronic trauma results from repeated or ongoing incidents such as domestic violence, abuse, or war.
– Complex: Complex trauma results from exposure to varied and multiple events, typically from events experienced earlier in life impacting the development of sense of self.
Trauma is very individualized:
– Not everyone experiences trauma in the same way, we cannot put trauma in a single box.
– Something that is traumatic for one experience may be something that doesn’t even phase another person. It just depends on our history, what we’re going through, what our experiences are.
Symptoms of Post Traumatic Stress Disorder (PTSD):
Just because you experience a traumatic event does not always mean you will have PTSD. In order to be diagnosed with PTSD, there must be the presence of one or more of the following intrusive symptoms associated with the traumatic event, after it has occurred.
Recurrent and intrusive symptoms:
– Recurrent and intrusive distressing memories of the traumatic event that happens involuntarily.
– Recurrent and distressing dreams in which the content and/or affect of the dream are related to the traumatic event.
– Flashbacks in which the individual feels or acts as if the traumatic event were recurring.
– Intense or prolonged psychological distress when exposed to either internal or external cues that symbolize or resemble an aspect of that traumatic event.
– Marked physical / bodily reactions to internal or external cues that symbolize or resemble an aspect of the traumatic event.
Avoidance symptoms:
– Persistent avoidance of stimuli associated with traumatic event, beginning after the traumatic event occurred, evidenced by one of the following:
a. Avoidance of distressing memories, thoughts or feelings about or closely associated with the traumatic event.
b. Avoidance of external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts or feelings about or closely related to the traumatic event.
Negative alterations in cognitions and mood associated with traumatic event, beginning or worsening after the event has occurred, evidenced by 2 or more of the following:
– Inability to remember an important aspect of the traumatic event, typically due to dissociative amnesia.
– Persistent or exaggerated negative beliefs or expectations about oneself, others, or the world (eg: “I am bad.” “No one can be trusted.” “The worst is completely dangerous.” “My whole nervous system is permanently ruined.”)
– Persistent, distorted thoughts about the cause or consequences of traumatic event that leads the individual to blame themselves.
– Persistent negative emotional states such as fear, horror, anger, guilt, or shame.
– Markedly diminished interest or participation in significant activities.
– Feelings of detachment or estrangement from others.
– Persistent inability to experience positive emotions such as loving feelings, satisfaction, inability to experience happiness.
Marked alterations in arousal and reactivity associated with the traumatic event, beginning or worsening after the traumatic event occurred. This can look very different in different people:
– Irritable behavior and angry outbursts (with little or no provocation) typically expressed as verbal or physical aggression toward people or objects
– Reckless or self-destructive behavior
– Hyper-vigilance
– Exaggerated startle response
– Sleep disturbance
– Problems with concentration
Symptoms must fulfill the following criteria to be diagnosed as PTSD:
– Duration of the disturbance is more than 1 month
– Disturbance causes clinically significant distress or impairment in the social, occupational, or other important areas of functioning
– Disturbance is not attributable to the physiological effects of a substance or another medical condition.
Sometimes, the symptoms may not happen right away and have a “delayed expression” even 6 months after an event. Or people may have dissociative symptoms and think it is not real or disassociate themselves from the event as if they are ‘watching’ things happen and not addressing it.
Important to note: Even if we experience something traumatic we may not show symptoms congruent with PTSD. There are other trauma / stressor-related diagnoses that could come up after a traumatic event such as acute stress disorder, adjustment disorders, and more.
The brain’s response to trauma:
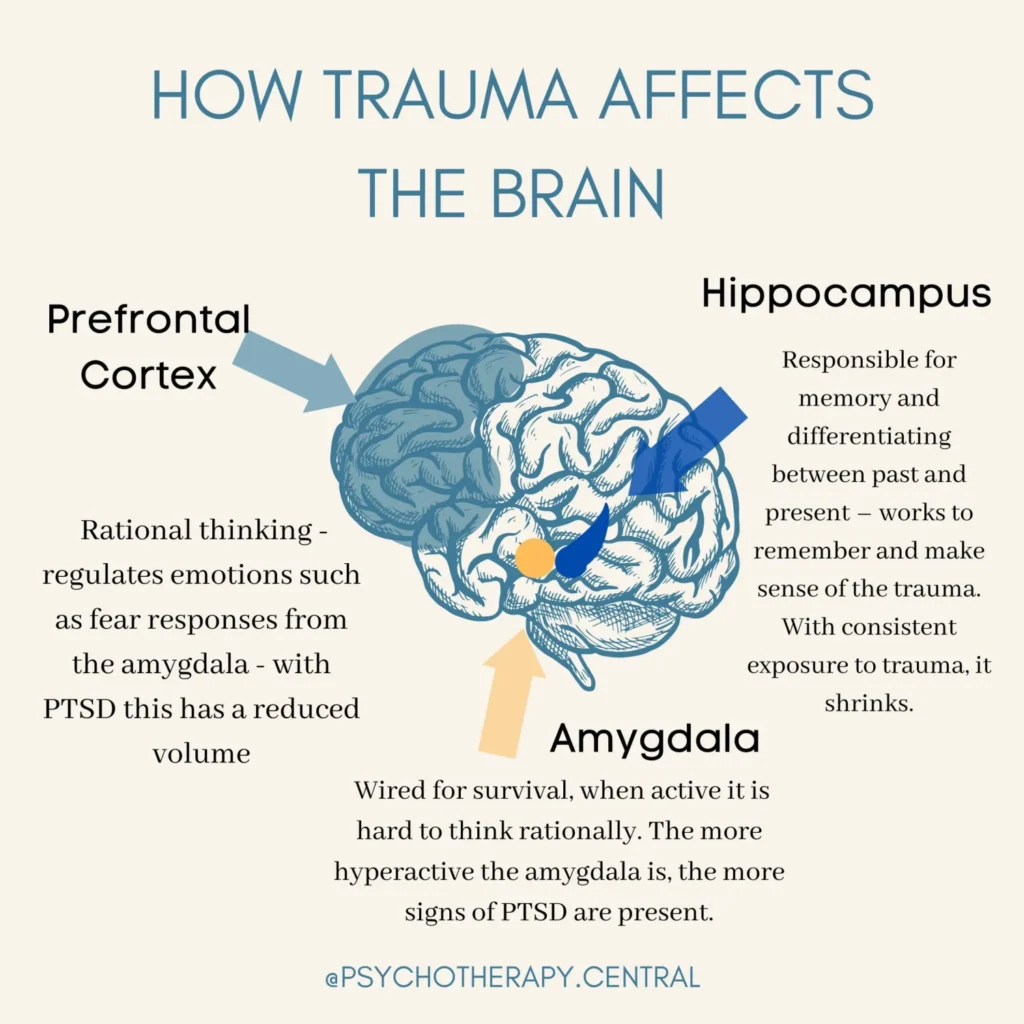
Trauma mainly affects three important parts of your brain:
1. The amygdala, which is your emotional and instinctual center
2. Hippocampus which controls memory
3. The prefrontal cortex, which is responsible for regulating your emotions and impulses.
All three parts work together to manage stress. When we are met with trauma, these three pieces of our brain are working overtime – our brain becomes more reactive, the past becomes present, and we become hypervigilant. It is hard to manage this stress in an effective way.
The body’s response to trauma
We have to remember that our body experiences trauma as well and when something happens that make us relive our trauma, we may experience the following:
– Fight or Flight Mode: an automatic physiological reaction to an event that is perceived as threatening where your body experiences increased heart rate, increased respiration rate, flushed or pale skin, dilation of pupils as
you scan your surroundings. Fight mode means you have a desire to strike out and hit / kick / punch, while flight mode means you feel the need to run or feel restlessness
– Freeze Mode: an automatic physiological reaction where the person feels stuck in their body, feeling stiff, cold, numb, restricted breathing or holding of breath, sense of dread)
– Loss of senses
– Migraines
– Asthma Attacks
– Alexithymia (where a person has difficulty in identifying and expressing their emotions).
Consequences of unresolved trauma and why it is so important to get the help we need:
Some people may rationalize their trauma and PTSD and say “oh, this isn’t so bad” or say something along the lines of “other people have it worse than me.”
Some of the risks of pushing our trauma aside may lead to the following issues in our lives:
– Relationship issues: Trauma tends to impact our ability to have healthy relationships. Those who experienced trauma for example may have difficulty trusting others, or understanding what is safe and what isn’t.
– Substance abuse / addiction: Those who experienced trauma may turn to substances to alleviate the pain.
– Severe mental health issues: Those who experience trauma may cause or exacerbate other mental health issues such as depression.
– Permanent damage to the brain: Trauma changes our brain because our brains are working overtime to process trauma and handle stressors.
– Work challenges: Trauma tends to impact our ability to do our job at work, as those processing trauma can have issues with focus, concentration, panic attacks, and more.
– Anger issues: Trauma can lead to higher levels of tension and arousal which becomes our ‘normal state.’ Being on edge can lead us to be more irritable.
– High risk behaviors: Trauma causes people to turn to high-risk methods to cope with stressful situations that are unsafe.
– Generational trauma: A lot of times we can pass down certain traits to our children and grandchildren if we are not thoughtful of seeking help.
If somebody else in our life has experienced trauma, how can we help them?:
Do not just say to them “It will be fine, shake it off, don’t worry, it will all be okay.” At this moment the person does NOT feel this way and you may inadvertently invalidate the depths of what they are feeling.
Instead, provide support in a way that shows curiosity and compassion. If we tell them “you will be fine, don’t worry” you are invalidating what they are experiencing. Come at them with a place of curiosity: “How was that experience for you? What was that like? I want you to know that you are not alone.” Gently encourage them to seek professional help if they are not already.
Common Trauma Informed Treatments:
Cognitive Behavioral Therapy: a common form of talk therapy that helps you identify negative or unhealthy types of thinking, and tackle negative reactions and behaviors resulting from this type of thinking.
Trauma Focused Cognitive Behavioral Therapy: therapy that addresses the mental health needs of children, adolescents, and families suffering from early trauma, where cognitive behavior therapy is employed to help tackle and sort out distorted, unhealthy types of thinking and its negative reactions and behaviors.
Eye Movement Desensitization and Reprocessing (EMDR): therapy that was designed specifically for treatment of PTSD that focuses directly on the memory of the traumatic event – this is based on the belief that the patient has not adequately processed the memory of the traumatic event leading to triggers and stressors of PTSD.
Narrative Exposure Therapy: this is a treatment used typically for individuals experiencing complex and multiple traumas where patients work with the guidance of a therapist to establish a narrative of their own life which includes their traumatic experiences while also including positive events.
Seeking Safety: this therapy is typically employed when addressing co-occurring PTSD and substance abuse, in which a manual is used and followed to ensure that the treatment follows the same steps for each session and combines CBT and psychodynamic therapy (in which the patient explores the past).
Neurofeedback: A noninvasive procedure that observes the patient’s brainwaves in response to various visual, video, or auditory stimuli and provides real-time feedback to the patient. This helps the patient gain back control over certain bodily functions that were involuntary triggered from stressors.
Somatic therapy: because trauma can be damaging to and ‘stored’ in the body, this type of therapy seeks to connect a person’s mind and body together, help individuals clear their minds and connect to their own bodies, and to apply both psychotherapy and physical therapies.
Trauma and the Gospel:
If you have experienced some sort of trauma, these are some things you can speak to with your therapist. Our traumas are so individualized so we want to make sure we have a few different options.
If you are undergoing trauma, have you asked one or more of these questions?:
– “Why me?”
– “Why is this happening?”
– “Where was God when this was happening?”
– “I am a good Christian, what did I do wrong?”
– “Why is God punishing me?”
– “If God loves me, why would He let this happen to me?”
– “If God is good, why is there so much evil in the world?”
– “If God cannot stop evil and suffering in the world, is he really All powerful?”
– “If God can stop evil and suffering, and chooses not to, he may be all powerful but is he actually GOOD?”
Trauma is not a new concept. There are many examples of Christians experiencing trauma in the Bible. As soon as sin was introduced to the world by Satan, trauma became an ever-present feature.
What does God say to his children, to us, who are undergoing trauma and trauma survivors?
The promise is not that we will never experience suffering or experience trauma, but that He will always be with us. Satan uses trauma as a tool to deceive us, to make us think God has abandoned us and cause us to stay away from God. In fact, during these times we need God more than ever. Satan’s lie is that we will never recover, never heal, and always despair and not see the light of the Lord.
However, it is important to know God’s truth and promise revealed in the Bible in the book of Isaiah. When we suffer and experience trauma with God, we know that the trauma will not break us. Jesus died and rose again to break us free from the original sin and the bondage of Satan that led to all the suffering in life. “Fear not, I have redeemed you. When you pass through the waters, I will be there. When you walk through the fire, you shall not be burned. Neither should the flame kindle upon you.” Isaiah 43
For those suffering and despairing today, note that some of God’s most beloved also underwent trauma and despair. Job, King David, Moses, Naomi were all beloved children of God that experienced death, famine, illness, hopelessness. But God was always with them, healed them, blessed them, and had an amazing purpose for them. This is something we, too, can experience as well.
Enjoyed our blogpost? Subscribe to our newsletter for more resources on mental health and integrating the Gospel message in your healing journey.
If you found our resources useful, please consider donating to Oak Health Foundation, which is a 501(3)c nonprofit dedicated to providing resources regarding holistic mental healthcare and subsidized treatment for those in need.