Bipolar disorder has a lot of stigma attached and a lot of misunderstandings surrounding it. Today in this post we’d like to address:
– Exactly what Bipolar Disorder is and what it looks like
– Four types of Bipolar Disorders
– Mania and hypomania – what is the difference?
– Depressive episodes and mixed episodes
– Other important facts about Bipolar Disorder
– What treatment looks like
– How finding hope in Jesus can help with recovery
Bipolar Disorder – What is it?
Previously known as Manic Depression, re-named in 1980 – one of the benefits of this change is the recognition that the illness isn’t as black and white as we once thought. Bipolar Disorder is a mental health disorder associated with episodes of intense mood swings, ranging from depressive lows to manic highs.
The Four Types of Bipolar Disorders:
There are four types of bipolar disorders:
Bipolar type 1: This is what we typically think of when we hear the term ‘bipolar disorder’ – manic or mixed episodes lasting at least one week, or manic symptoms that are so severe that a person needs medical care / hospitalization. Individuals with Bipolar I are symptomatic 47% of the time, with depressive weeks outnumbering the manic / hypomanic episodes by 3:1.
Bipolar type 2: Instead of full manic episodes, people with Bipolar type 2 experience hypomania rather than mania – a persistent, abnormally elevated, or irritable mood accompanied by unusually increased activity for most of the day over at least 4 days, as well as depressive episodes where they experience a low mood, sadness, emptiness, hopelessness. Clients with Bipolar type 2 are symptomatic 54% of the time.
Cyclothymia: Subclinical hypomania that is a rare mood disorder. It causes emotional ups and downs, but not as extreme as those with Bipolar 1or Bipolar 2 disorder. Symptoms are still out of character and causing impairment in someone’s life.
–
Bipolar Disorder-unspecified: symptoms of bipolar disorder that don’t fulfill the criteria necessary for a diagnosis of any of the other categories of Bipolar Disorder, and symptoms are clearly out of character and causing significant impairment in someone’s life.
Mania and hypomania, and what’s the difference?
Both manic and hypomanic episodes require the presence of at least 3 of the following symptoms during the mood disturbance for diagnosis:
– Inflated self-esteem or grandiosity
– Decreased need for sleep
– Increased talkativeness or pressured speech
– Racing thoughts or flights of ideas
– Distractibility
– An increase in goal-directed activity or psychomotor agitation
– Excessive involvement in activities that have a high potential for painful consequences.
Although the symptoms are attributed to both mania and hypomania, there is a change in functioning that is uncharacteristic of the individual when not symptomatic: hypomania leads to less impairment than mania or even a perceived improvement in functioning.
Hypomania does not require hospitalization, and does not involve psychosis (where contact is lost from external reality) that may be present in a manic episode.
Mania often will lead to hospitalization because individuals are experiencing something so intensely, that they have a difficult time controlling their emotions and actions. Oftentimes, manic episodes will have an element of psychosis to them where some patients will actually forget what actually happened, and the consequences of their actions, once the episode is over. There can be high potential for very harmful consequences during these manic episodes. For example, a patient during a manic episode may spend hundreds of thousands of dollars on a credit card impulsively, or having unprotected sex, or engaging in other destructive behaviors without thinking much about their actions and consequences. Hypomania is not as intense as that. It is less likely that it will lead to hospitalization or have severe effects.
Reasons why Hypomania is a Double-Edged Sword
Hypomania can be a double-edged sword that can be complex to treat for the following reasons:
- People can enjoy experiencing feeling happy and energetic, especially if they spend a lot of time in depressive episodes. Those with hypomania may think to themselves: “If I am feeling depressed for most of my life and can experience bursts of energy and excitement, I would want to stay there.”
- People often feel more productive and creative during hypomania. People who are artists or creatives will think that their brain will not function normally if they are not ‘flying high’ and are on medication. Thus, having patients actually wanting and following treatment regimens for hypomania can be difficult.
- Hypomanic episodes can potentially turn into full-blown mania if left untreated. If we are not managing hypomania or mania, that can definitely lead into a crash into depression – especially when we realize the effects of our behaviors from a manic episode.
- At its extreme, mania can be dangerous and destructive. Again, it is important to reiterate that for some patients who experience a manic episode, it may be difficult for them to remember what exactly happened during that period because our brains are not functioning normally.
- The more manic / hypomanic episodes individuals have, the more cognitive decline they will typically experience as they get older with increased risk for dementia.
Depressive episodes for those with Bipolar Disorder: what does this look like?
People with bipolar disorder will experience manic or hypomanic episodes followed by a period of a depressive episode. These are called the ‘highs and lows.’ It can also happen at the same time.
A person may be experiencing the depressive phase of bipolar disorder if at least 5 of the following symptoms are present for at least 2 weeks and experienced on most days:
– Depressed mood
– Loss of interest or pleasure in activities that used to be enjoyable
– Weight loss or gain
– Difficulty sleeping, or sleeping too much
– Apathy or agitation
– Loss of energy
– Feelings of worthlessness and guilt
– Inability to concentrate
– Thoughts on suicide
Mixed Episodes: We can also experience both mania/hypomania AND depression at the same time.
This occurs in 10-30% of cases, with studies suggesting mixed features are indicative of a more severe and disabling course. This does not mean it is untreatable! However it is especially important for people to be aware of this fact because there is a heightened risk of suicide in this state.
When does Bipolar Disorder start?
Research shows that the average age of onset is late teens between 50-66% experiencing onset of bipolar disorder before age 19 to early 20s. Those with an earlier age of onset are typically associated with a more severe course of illness. According to Post’s (1992) kindling hypothesis, major life stress is required to trigger initial onsets and recurrences of episodes, but successive episodes become progressively less tied to stressors and may eventually occur autonomously. It is very important to seek help and support as soon as possible!
What is it like for people with Bipolar Disorder?
Research shows that people with bipolar disorder will generally:
– Have higher unemployment rates as it is difficult to hold down a job
– Lower wages as a result of higher unemployment
– Lower levels of educational attainment and completion
– Higher arrest rates due to manic episodes
– Higher hospitalization rate due to manic episodes
– Rates of substance abuse and dependence – sometimes substances will help them ‘mellow out’ a bit or help them forget about the emotional turmoil they are experiencing.
– Increase rates of divorce because people who struggle with bipolar disorder will have a hard time connecting with a partner in a stable way.
We really want them to address all of these challenges, and help our patients be able to have healthy relationships.
The link between Bipolar Disorder and Suicide.
6-7% of those diagnosed with bipolar disorder will experience death by suicide. It is therefore SO important for clinicians to understand this and educate our patients and their loved ones that this is a real issue and something we pay close attention to and approach with care and love.
Why is there such a stigma for those with Bipolar Disorder? And why is it important to get rid of this stigma?:
It is because the symptoms that people with Bipolar Disorder experience can be super intense and show itself very intensely, so that surrounding people who may witness this may judge –– and this creates stigma. The intensity of the symptoms tend to lead this to judgment and stigma by others.
When Type 1 and even Type 2 patients enter their manic or hypomanic episodes, it seems very erratic and out of character to friends and family witnessing these episodes and thus they can feel taken aback. One moment, the patient can be very happy, energetic, and productive and then suddenly switches or “swings” (this is why we call them mood swings) to a depressive disorder and they are suddenly in bed all the time and melancholic. The friends and family who witness this are taken aback and ask “what are you doing? Why are you like this?”
These erratic switches associated with this disease also have people casually insulting and commenting behind people’s backs who experience even normal highs and lows at home or in the workplace as “bipolar.” Thus, over time this disease has become misunderstood and stigmatized.
Treatments for Bipolar Disorder
What are the different types of treatment for bipolar disorder?:
1. Psychoeducation: we want people to be aware of the struggles and challenges of bipolar disorder, and we want to reduce the stigma! How many times have some of us said “I’ve felt so bipolar today?” Let’s talk about that. What does that actually mean? It is a way to say we are experiencing some ups and downs in life, but we have to realize it is a very intense statement because there are people who are truly experiencing this, and anyone casually saying this may invalidate what they are going through.
2. Cognitive behavior therapy (CBT) / dialectical behavioral therapy (DBT): DBT works wonderfully with people who struggle with bipolar disorder as they have difficulty managing their extreme highs and lows and regulating their emotions.
3. Family focused treatment: Our patients need a strong support system. We want the family to be informed and have the tools to support their loved ones with empathy and grace, and help create peace in their lives.
4. Stress/lifestyle management: The more we can reduce stress in somebody experiencing bipolar disorder, the more they will be able to manage their emotions.
5. Comorbid disorders: This is when two disorders or illnesses occur in the same person, at the same time. For example, as mentioned before, those with bipolar disorder may experience substance abuse disorder as well to “mellow out” their emotional intensity and/or forget about their troubles.
6. Medication: This is a big one and a cornerstone of treatment for bipolar disorder. Of course CBT and DBT are very helpful, but sometimes the brain and our neurotransmitters need the help to effectively use the skills taught in CBT and DBT.
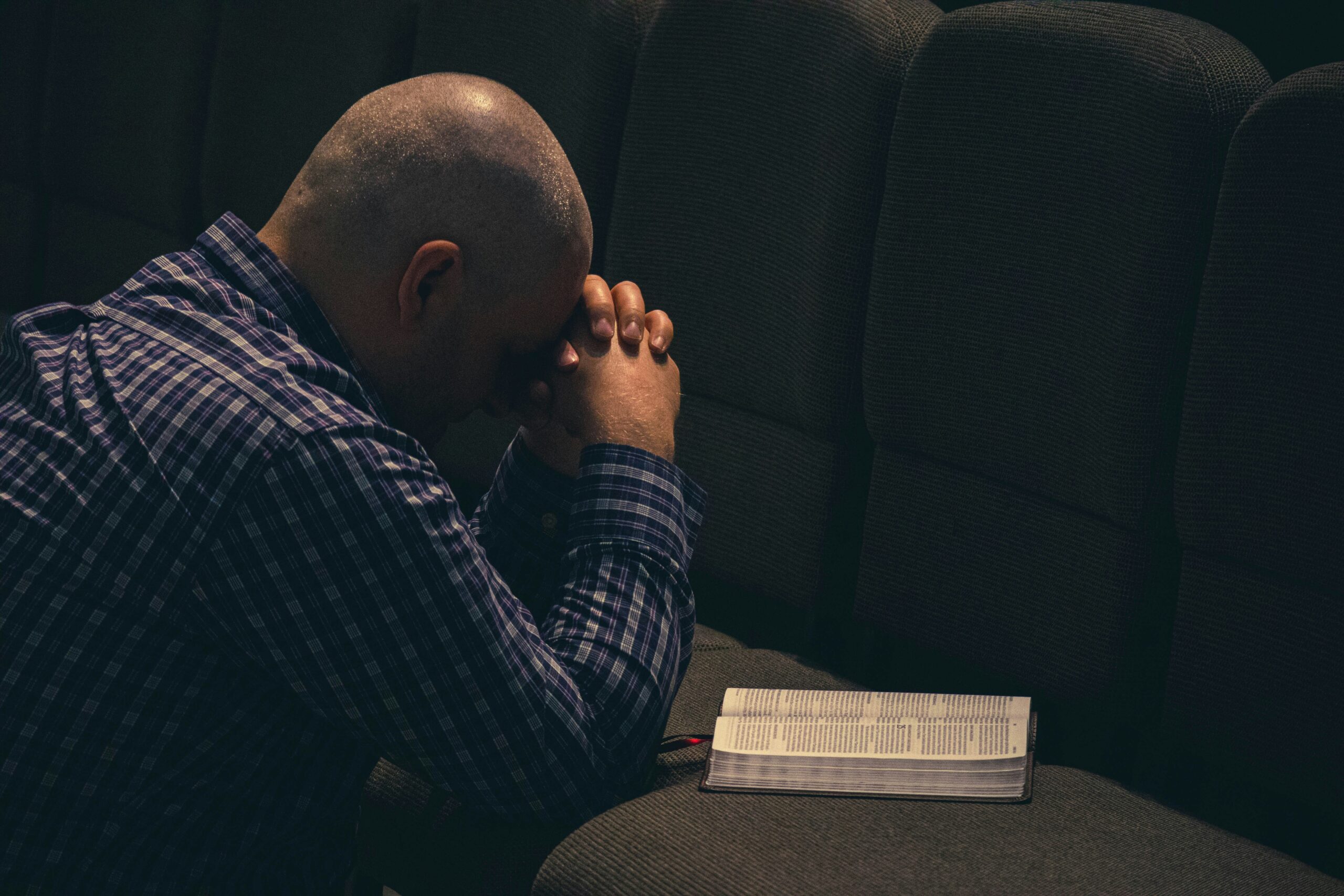
How Jesus can bring hope to those with Bipolar Disorder:
Many of our patients, once diagnosed, their illness becomes a huge part of their identity. They will say “I am bipolar” or “I am depressed.” They will also ask “Why is this happening to me?”
What if we were able to shift this self-identification to include: “I am a beloved child of God?”
What are the possibilities when we shift our thinking to “I am a beloved child of God?” That means we also may feel worthy of healing. And therefore go seek therapy and the treatment that I need, find trusted practitioners, and remember that God’s love is always there even when we are experiencing the darkest of times.
When we understand that we are a beloved child of God, then we realize we are worthy – worthy of meaningful connections, healing, forgiveness, redemption, happiness. And that we are not without hope. Nothing can separate us from His love, not even the worst disease or disorder that we may go through, as stated in Romans 8:38-39: “I am convinced that neither death nor life, neither angels nor demons, neither the present nor the future, nor any powers, neither height nor depth, nor anything else in all creation, will be able to separate us from the love of God that is in Jesus Christ our Lord.”
It is easy and understandable for patients going through Bipolar Disorder to ask “Why am I suffering? Why am I going through this?” We have to stand firm and hold faith. We have to realize that God has put us on this earth for a purpose. When we feel lost, especially as we are going through the rollercoaster of extreme highs and lows, it is important to remember: not even a debilitating challenge such as bipolar disorder will not separate us from Him.
God is also in favor of treatment. God wants us to take care of ourselves! Healing allows clarity of the mind to know and experience His Love.
You must remember: You are priceless – fearfully and wonderfully made. God shaped and modeled you in your mother’s womb. God created you in his own image. You were created, redeemed, and are deeply loved and valued by God. How do we know that? Because Jesus died for you and me!
Enjoyed our blogpost? Subscribe to our newsletter for more resources on mental health and integrating the Gospel message in your healing journey.
If you found our resources useful, please consider donating to Oak Health Foundation, which is a 501(3)c nonprofit dedicated to providing resources regarding holistic mental healthcare and subsidized treatment for those in need.