What is Obsessive Compulsive Disorder?
Obsessive Compulsive Disorder is when a person experiences intrusive, unwanted thoughts (the obsession) and feels the urge and the need to perform certain routines or actions (the compulsion) to relieve the emotional and
psychological distress the person feels due to their obsessions.
OCD in two components: Obsessions and Compulsions
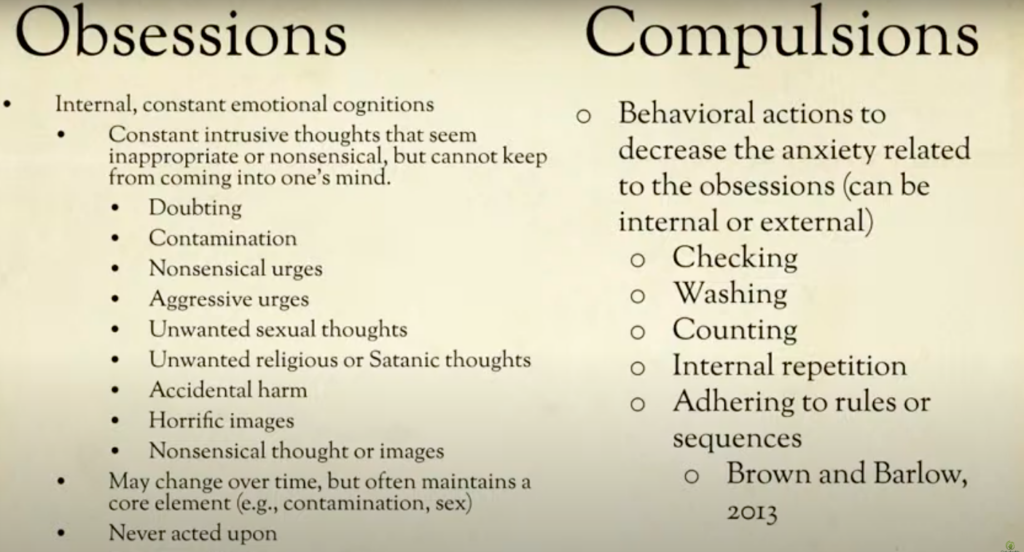
Typically we think of OCD in two components: obsessions and compulsions.
Obsessions are constant, intrusive thoughts that seem inappropriate or nonsensical, but it continues to enter one’s mind. It’s not just once or twice a day but dozens, hundreds to thousands of times a day. It is a repeated, continual thinking pattern.
They typically fall into different categories, some common ones include:
– Self-doubt, for example thinking “Did I close the garage door? Did I turn the stove off? Did I lock my door” the entire day, every day while at work, instead of forgetting about it and moving about their day.
– Contamination, where a person thinks they themselves are contaminated and cannot stop the urge to wash their hands raw or cleaning themselves.
– Unwanted religious / moral thoughts, such as praying excessively or engaging in rituals triggered by a fear that they will be punished or their life will go awry.
– Order and symmetry, such as when a person is obsessed with order or symmetry and cannot stop arranging or ordering things.
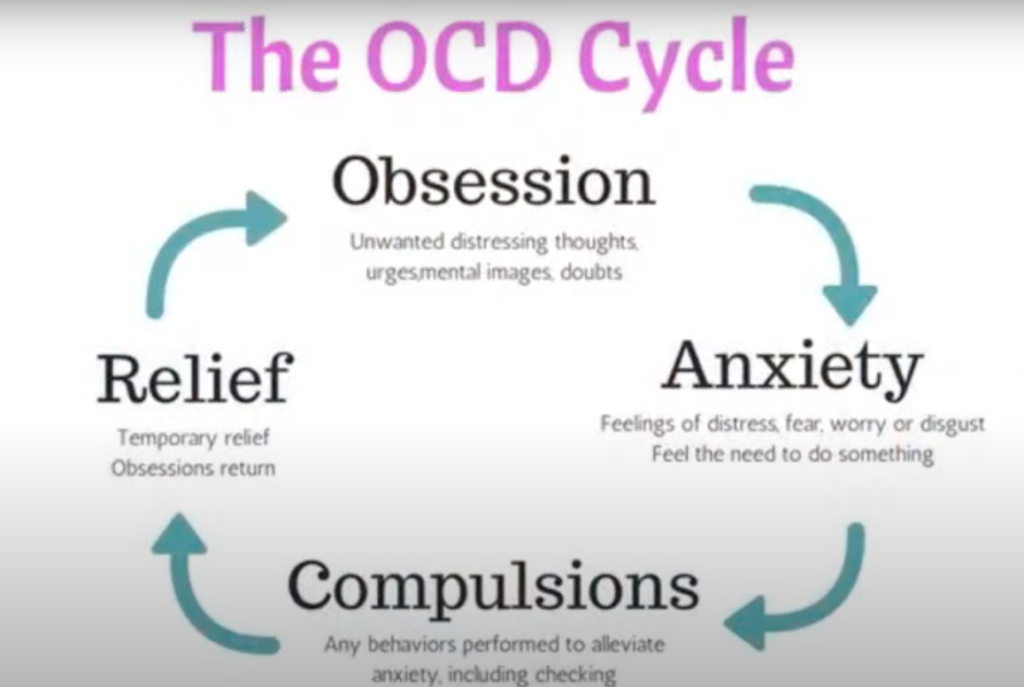
Obsessive Compulsive Disorder involves a vicious cycle where a person is obsessed with something that doesn’t “feel right” which then leads to anxiety. This anxiety then leads to a compulsion which is an action that is supposed to alleviate this anxiety.
Sometimes the compulsion is related to the obsession, such as when a person thinks they are ‘germy’ and ‘contaminated’ and cannot help but wash their hands repeatedly.
Other times, the compulsion does not seem to be related to the obsession and may not seem logical on the surface level – for example, a person may feel a compulsion to keep their desk arranged in a certain way because they think it will prevent their parent from having a heart attack.
These are the hallmarks of OCD.
Diagnosing Obsessive Compulsive Disorder
When diagnosing and treating obsessive compulsive disorder, we look for the following:
– Level of interference and distress: How much is the obsession and compulsion interfering in the person’s life? If someone is spending more than one hour a day planning around their OCD or acting upon their OCD, they may have a disorder. Typically when someone is diagnosed with OCD, their obsessions and compulsions impact their relationships at home, school, and at work.
– How often can obsessions/compulsions be resisted? There is a difference between someone who may sometimes have nagging thoughts for the short-term to someone who has recurring, intrusive thoughts that causes significant distress and anxiety and will not go away until some action is carried out.
– The disturbance / behavior cannot be attributed or explained by other reasons or symptoms of another mental disorder such as drug/substance abuse, generalized anxiety disorder, body dysmorphic disorder etc.
Treatments for Obsessive Compulsive Disorder:
When treating obsessive compulsive disorder, clinicians will tend to combine psychotherapy and medication, such as Luvox which is the one most often seen and prescribed for this type of disorder. Medication alone may help “turn down the volume” of the obsessive thoughts and the anxiety, but the gains are often lost when the patient goes off the medication.
Cognitive behavioral therapy (CBT) is commonly used for treatment as well, as it can help the patient understand and break free from the vicious cycle / feedback loop between obsession, anxiety, and subsequent compulsions. Psychotherapy helps patients learn a tool to help manage their obsessions with or without taking a pill.
Cognitive approaches for OCD: How we help patients “think through” their obsessions:
During psychotherapy, clinicians will help the patient tackle the intrusive thoughts, break it down, and finally try to break away from those thoughts. For example, if someone is obsessed about not touching doorknobs for fear of contracting a horrible disease such as AIDS, we break this thought down together and ask “does this factually make sense? How often do we hear about AIDS on doorknobs and people catching AIDS from doorknobs and that sort of surface? What does my data say? say?” We pull apart OCD thinking from logical thinking. We talk a lot about how to recognize when we are thinking logically, and when we are thinking illogically.
We also talk a lot about being “comfortable with being uncomfortable” by normalizing anxiety and discomfort in our lives. Our daily lives can sometimes be a bit stressful and anxiety-inducing. We have to acknowledge that we just experienced a global pandemic, there is high inflation that impacts our daily lives, there are geopolitical things beyond our control. Of course everyone feels anxiety and discomfort from time to time. We have to normalize that it is OK to be uncomfortable instead of immediately thinking “I must get rid of this anxiety right now and must do something right now.”
Exposure and Response Prevention (ERP):
Not only do treatments tackle the cognitions and thought processes behind OCD, they will typically tackle the behavioral aspect of OCD through exposure and response prevention.
With Exposure and Response Prevention we focus on helping the patients become accustomed to the things that they are fearful of through exposure, and help them realize that nothing catastrophic will happen.
For example, if someone is scared of dogs jumping on them and will engage in compulsions to avoid running into this possibility, we will first talk through this fear with the patient logically. Then we will start introducing them to situations where they will have to get used to the things that scare them and help them actively not engage in compulsive behavior.
With this patient, we will start with pictures of dogs and puppies, followed by stuffed animals. Then we start increasing that level of intensity to get them more comfortable with their discomfort, perhaps even taking them to a dog park. This helps normalize their anxiety and show them that it is OK to be scared and uncomfortable, but nothing catastrophic will happen. Patients will typically also have homework outside of their sessions where they will practice facing their fears, work through their thinking patterns and change the way they think and behave.
Case study of OCD:
Taylor is a 14 year old female who lives with mom during the week, father on weekends. She has constant obsessional thoughts and eight hours of rituals daily. She currently takes moderate medication for OCD that were not very effective.
Her obsession involves being afraid of contamination of “germs.” Ever since the global pandemic, the general concern for germs has shifted specifically to COVID concerns. She has constant concern about becoming infected, or infecting others. Initially it was simply a ‘quirk’ where she would sometimes take very long showers or wash her hands raw but she was still able to function well in school, and hang out with her friends. However during COVID-19 her fears escalated to a point where she was constantly concerned that contracting COVID would kill her, her parents, and/or her grandparents. It creates a lot of anxiety.
To decrease her compulsions and her anxiety, she is taking many more showers, constantly washing her hands, trying to use bleach to clean herself, constantly changing her clothes, using sticks to move objects, avoiding contaminated areas of the house near thresholds, as well as yelling at friends and family.
What do we do about this? We separate her thinking from her OCD thinking. We separate logical thinking vs. emotional thinking. We ask her: where is the data? What do health experts say about touching objects when outside? If your family members are touching doorknobs in the house and not getting sick, why would you? What does the data tell me?
We help the patient take a data-driven approach instead of a theory-driven approach (my theory is that touching something will give me COVID).
We then begin exposures for her including:
– Touching contaminated objects in the house repeatedly and then touch her arm or her face and get used to that anxiety. The anxiety level goes up, then after 10-15 minutes the anxiety levels drop down.
– Saying out loud verbal statements repeatedly such as “I have COVID” or “I gave my brother COVID” to help her get used to these statements and realize it’s not true anymore.
The goal of exposure therapy is to desensitize the patient to thoughts regarding contamination, normalizing having the scary thoughts while recognizing the issue is OCD. The more desensitized we become, the less scared we become.
Treatment is very important because only 1% of the cases will go away on its own.
Religious Thought Cycle vs. Gospel Thought Cycle
In some ways, the religious thought cycle is very similar to the vicious cycle of OCD
In the “religious thought cycle” begins with my decision. I will decide to follow this or that religion, or philosophical rules or laws. Usually the goal is to attain salvation, enlightenment, or blessings by following the laws by performing rituals, believing a set of beliefs, living a certain lifestyle. Typically I am expected to try my best. However, like any human being we will make mistakes and fail at times (sometimes it is considered falling into sin). What do we do when that happens? We will try harder to keep the law. To follow the rules. To continue doing the rituals such as praying, giving alms, whatever the religion demands. And we will continue to try and try, make mistakes, try harder, do better. In this religious cycle, there may be two results that come out of it:
– Success: The person may perceive themselves to be very successful at adhering to the law / religion and may feel happy and proud of themselves. There is nothing inherently wrong with this. However, this may also cause the person to judge or compare with others.
– Failure: On the other hand, the person may feel as though they are making very slow progress in being a “good person.” The person feels guilty or discouraged, and this can also lead to despair.
The Gospel Cycle:
The gospel cycle on the other hand shifts our perspective from ourselves, and our actions to God and the good news message.
Ephesians 2:8-9 says:
“For by grace you have been saved through faith. And this is not your own doing; it is the gift of God, not a result of works, so that no one may boast.”
In this cycle, the starting point is God’s grace. We are encouraged to understand and believe and enjoy the Gospel, the good news that we are saved from sin and spiritual death through God’s grace. We just have to receive and believe it. In this cycle, we will still make mistakes, fail at times, and fall into sin again. In this gospel cycle, the encouragement is to REALIZE that we need Jesus, that we always need Jesus.
Galatians 2:16 says:
“Know that a person is not justified by the works of the law, but by faith in Jesus Christ. So we, too, have put our faith in Christ Jesus that we may be justified by faith in Christ and not by the works of the law, because by the works of the law no one will be justified.”
My identity should not be based on my ability to keep the law but realizing, understanding, and believing in the Gospel. Even if inevitably fall into sin, come into hardship, make mistakes, we need to keep on remembering the gospel and keep on receiving God’s grace.
– Success: When a person is in the Gospel cycle and experiencing ‘success’ and feeling a strong relationship with God, this will lead to thanksgiving, giving glory and credit to God. Because of this, this person would not judge others.
– Failure: When a person is in the Gospel cycle but is experiencing failure and hardships, and feeling as if their relationship is not as strong, my encouragement is that this will hopefully increase the person’s hunger to know Jesus and to know that God’s plan and timing for you is perfect.
We hope that you can take away from all this that even though you are experiencing and combating OCD and may be going through a vicious feedback loop of anxiety, God is here for you and he has a plan for you.
Enjoyed our blogpost? Subscribe to our newsletter for more resources on mental health and integrating the Gospel message in your healing journey.
If you found our resources useful, please consider donating to Oak Health Foundation, which is a 501(3)c nonprofit dedicated to providing resources regarding holistic mental healthcare and subsidized treatment for those in need.